From Trauma to Transplant
Rosheen’s Long Journey to Wellness
March is National Kidney Month, and from presentations before Congress to Kidney Walks throughout the country, many are focused on advocacy, improving care, and raising awareness of how kidney disease affects hundreds of millions worldwide.
One of those affected is Rosheen, a travel enthusiast and grandfather from Sacramento, CA. And his story isn’t just one in a million – it’s one of a kind.
Heart failure? Check. Kidney Failure? Yes. Dialysis? Affirmative – in-center, peritoneal dialysis, and home hemodialysis. Transplants? Two. It sounds like the stuff of fiction, but this has been Rosheen’s world since day one.
A rough start
“I had a heart murmur since birth and developed an enlarged heart,” he explains. “At one point, I caught a virus, and it shut down my heart, kidney, and lungs. I actually passed away, but God allowed me the opportunity to come back.”
Early in his life, doctors said Rosheen’s heart and/or a kidney would fail at some point, and in 2009 the second half of that prediction came true. It was a blow to his lifestyle, plans for the future, and typically positive outlook.
A change of plans
“I was a project manager working 65 hours a week. I was being mentored. I wanted to become a GM,” Rosheen remembers. “My primary care physician (PCP) said ‘You can’t put your health on the back burner. As of today, you are retired, and you have to focus on this.’ That day the ambition and the goals had to change to surviving.”
Rosheen’s grandmother had passed while on dialysis and he was determined to get through this ordeal. He researched. He read. He talked to patients. He gathered information.
“I’ve always been a spiritual person, I trust God in all things,” says Rosheen. “I had to make a call. Either it was going to be the death of me or it was going to be the reason I would fight to live.”
A change in focus
His nephrologist got Rosheen on the transplant list, and recommended he lose weight. The hope was that shedding some of his 363 pounds might put Rosheen’s kidneys in remission and delay dialysis. He considered gastric bypass surgery, but his PCP shared a photo taken just a year before, when the doctor was 100 pounds heavier. He told Rosheen he didn’t need surgery, just a lifestyle adjustment.
“It’s like he did a Jedi mind trick to me,” says Rosheen with a laugh. “He said, ‘Right now what you’re doing is not working. So do the opposite. Give up soda and chips. Eat healthy.”’
That day, Rosheen emptied his snacks into the trash. In just two weeks, he lost 12 pounds and kept losing. It was a victory, but soon he began feeling the effects of kidney failure. He was lethargic and “felt like there was a dark cloud just smothering me.”
That began a series of procedures, therapies, surgeries, ups, and downs that would last several years.
Treatments Begin – Hemodialysis
First came a fistula and PD catheter (done at the same time because the surgeon wanted him to have a back-up plan). Rosheen then started in-center hemodialysis – three days a week, five hours at a time. He said it was very good for him, and the clinicians and staff were encouraging, but the post-therapy recovery time was tough.
“I had to wait in my car for 45 minutes just to gather enough energy to make the fifteen-minute drive home,” he remembers.
Six months in, his vascular surgeon’s advice proved to be more of a prediction, when his fistula developed an irreversible clot.
Recovering His Freedom - Peritoneal Dialysis

With a catheter already in place, Rosheen trained for PD, and was able to go on a seven-day Caribbean cruise within a month.
“I loved PD because it gave me my freedom back,” recalls Rosheen. “You can do it at night, and you get up and you’ve got the day ahead. You can go out with friends. No one would even have known I was on dialysis.”
Six years passed, and Rosheen had to stop PD due to complications. The next step appeared to be transplantation. But while seeking medical approvals, his cardiologist told him he needed a heart as well as a kidney. He would have to wait.
“I had been on the list since 2009 and done everything to be a good patient,” Rosheen remembers. “It was like a kick in the gut.”
Staying the Course – More Frequent Home Hemodialysis (HHD)
With an unknown waiting period, it was time to consider a new form of treatment. His doctors explained that dialyzing more frequently may be able to help him manage his fluids and reduce pressure on his heart. They hoped his heart might go into remission, negating the need for a transplant.
Once again, Rosheen did his homework, learning all he could about HHD. He was nervous about self-cannulating, especially since he’d have to do so left-handed due to the failed fistula in his left arm.
“The first time I cannulated myself it was like confronting a spider or snake,” recounts Rosheen. “I said a little prayer … ‘Give me the courage to do this.’”
Rosheen learned to self-cannulate and finished his HHD training. To make things more comfortable at home, he set up a space with a big chair, a fridge, a heater, and a table for his cycler. Using a NxStage System One, he treated three hours a day, five days a week.
“I loved home hemodialysis,” he says. “A blessing for me was the improved recovery time1. I would literally get off the machine, get dressed and go to the gym. Home hemodialysis worked for me rather than me working for it.”
Heart Matters
While more frequent HHD helped Rosheen feel better2, he learned that he would still need a heart transplant. In March 2016 he was prescribed a left ventricular assist device (LVAD).
An LVAD is essentially a pump, surgically implanted just below a weakened heart, to help keep it functioning properly. The patient wears a harness or belt (24 hours a day) with battery packs and a controller, which are all connected to a power cord. The cord comes out of the abdomen and runs up inside the chest cavity to the pump.
Rosheen was told he needed to use this device until a heart became available. It also meant he spent time each week connected to and managing two different machines simultaneously.
Faith rewarded
With medical technology keeping him alive, Rosheen prayed and waited for an available heart and kidney. More than a year passed, as well as periods of hope and disappointment. Each time he seemed close, the door would shut.
Then something positive occurred. In the midst of a tragedy, there was Rosheen’s chance at a new life. He found himself on the phone with his ex-wife’s cousin, Cheryl. She asked him to come to the hospital as fast as possible. When he got there, Cheryl explained that her 23-year-old nephew was on life support, after a terrible motorcycle crash. Rosheen “hugged her and loved on her” and she walked him into the hospital.
A doctor greeted Rosheen and said “Brother, I’ve been doing this for 30 years. No one ever meets the donor.”
“I walked into the room and there’s this kid on life support,” Rosheen remembers with emotion. “I put my hands on him and prayed over him. Then I prayed with the family. Within 10 minutes, UCSF Medical Center calls me and tells me it’s a perfect match. I could have fallen over. It was the most excited and sad that anyone could be.”
The following Tuesday morning, Rosheen woke up for the first time in a long time, not connected to a machine. He also found out he would get to meet his first grandson, born premature just days prior.
“I was fighting for my life and he was fighting for his life,” recalls Rosheen. “The doctors allowed me to leave the hospital ahead of schedule so I could have the privilege of meeting him. That’s the reason I was fighting.”
 Paying it Forward
Paying it Forward
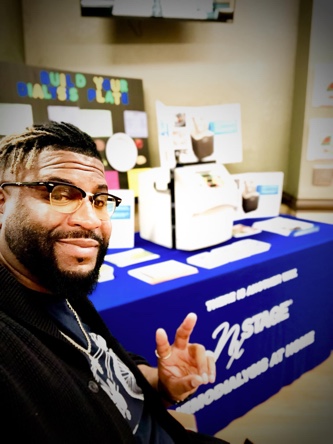
Three years later, when he isn’t traveling or spending time with family, Rosheen is still fighting – though not for himself. After all he has been through, he wants to share his experience with other dialysis patients as a NxStage Patient Advocate.
“I have literally gone thru everything a dialysis patient is enduring,” says Rosheen. “For me to be able to give the encouragement and experience to provide hope to each patient, is my willing, giving offering. I was in their shoes and, for me, being an advocate is like being a 911 call for patients in need of answers.”
Not everyone will experience the reported benefits of home and more frequent hemodialysis. All forms of hemodialysis involve some risks. When vascular access is exposed to more frequent use, infection of the site, and other access related complications may also be potential risks.





